Photo by The Hartford Courant
As the country continues in its struggle against the coronavirus, dozens of domestic companies have been racing to manufacture the first vaccine to be approved by the United States Food and Drug Administration (FDA). In the past few months, testing sites have opened around the country to support these companies as they enter the clinical testing stages for their vaccine candidate. On August 17, the Yale School of Medicine and Yale New Haven Hospital joined phase three of the vaccine trials for Pfizer’s BNT162b2 vaccine.
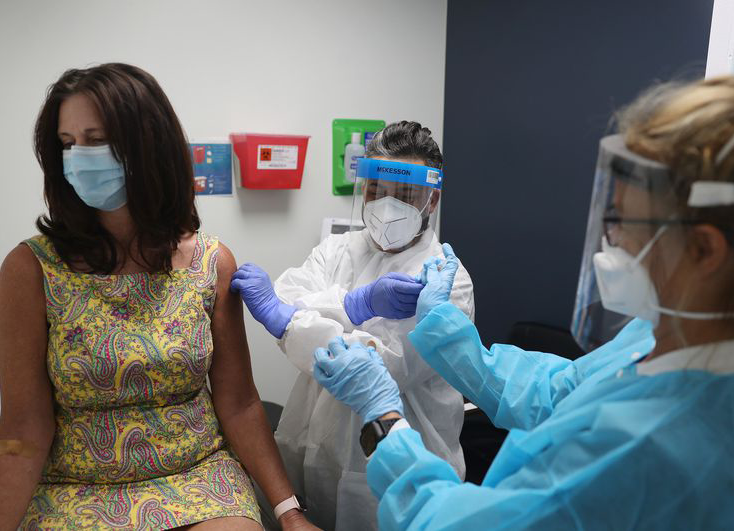
BNT162b2 is an mRNA-based vaccine manufactured by pharmaceutical company Pfizer with mRNA technology provided by German company BioNTech SE. Seeking approval for public distribution and use of their vaccine, Pfizer opened over 100 testing sites and recruited around 30,000 volunteers across the country for the vaccine’s clinical trials. As of August 26, over 400 volunteers had signed up for the study at Yale. After filling out paperwork on the Yale Center for Clinical Investigation website, volunteers begin their participation by receiving an injection and getting their blood drawn.
“You get an injection, and that injection is either the vaccine or placebo,” said Dr. Thomas Balcezak, Executive Vice President and Chief Clinical Officer at Yale New Haven Health. “It’s a randomized controlled trial meaning that…the patient doesn’t know what they get and the person who is administering [the injection] doesn’t know what [the patients] get.”
Three weeks following the initial injection, participants return for their second injection. Over the course of two years, these participants are scheduled to have four follow-up visits.
On September 12, Pfizer submitted an amended protocol to the FDA, expanding the trial to 44,000 people in order to include a more diverse population. “The proposed expansion would…include adolescents as young as 16 years of age and people with chronic, stable HIV (human immunodeficiency viruses), Hepatitis C, or Hepatitis B infection, as well as provide additional safety and efficacy data,” Pfizer wrote in a public statement.
Pfizer’s vaccine candidate utilizes groundbreaking techniques that are engineered to stimulate the body into creating coronavirus spike proteins, which the virus uses to enter cells. The immune system can then develop a defense against those proteins.
To receive approval from the FDA, the vaccine has to reach a threshold of 50% efficacy, meaning that the vaccinated population is at least 50% less likely to contract the coronavirus. Based on the vaccine’s preclinical trial profiles, Pfizer has high hopes that its vaccine will surpass this requirement. Dr. Albert Bourla, Chairman and Chief Executive Officer at Pfizer, said at the JPMorgan US All-Stars Conference, “We have a low threshold of 60% efficacy. FDA has asked [for] 50%. We’re a bar higher because we are very confident.”
Months into the pandemic, the coronavirus is still mutating into different strains. These constant changes have raised concerns about the potential efficacy of the vaccine. “No one really knows the answer to that question yet,” said Dr. Balcezak. “But, the [coronavirus’s] spike protein seems to be pretty consistent. This particular virus hasn’t mutated a ton…there is the hope that [we] are not going to need the new vaccines developed and that this vaccine will remain effective against it.”
The rush for an FDA-approved vaccine also generates concerns regarding the vaccine’s quality. Only in January did scientists discover the virus’s genome, yet in less than a year, nine vaccines worldwide are already in phase three testing. Furthermore, on September 15, Pfizer announced in an investors conference that some participants were showing mild-to-moderate symptoms including fatigue, headache, chills, and muscle pain. Data from these phase three trials is particularly crucial because they ensure that companies are certain about the safety of the vaccine prior to public release.
Even if a viable vaccine makes it onto the market, the public may be deterred from vaccination due to concerns about safety precautions and procedures performed by the vaccine manufacturers. “Right now, [the manufacturer’s] only requirement is to show the data to the FDA,” said Dr. Balcezak. “There are many who are calling for transparency in these trials.”
Dr. Bourla announced on September 14 that they plan on publicizing an estimated efficacy of the vaccine by late October. With 100 million doses set to be sold to the U.S. Health and Human Services Department and the U.S. Department of Defense (contingent on FDA-approval), the vaccine can potentially put an end to the pandemic. “[We] are going to have to make sure that it is safe. That’s the responsibility of the FDA. It’s the responsibility of the investigators, and it’s the responsibility of the manufacturer,” said Dr. Balcezak.




